ParaSahel – DIMAS
NTDs are persisting
WHO defines a group of 20 diseases as so-called neglected tropical diseases (NTDs). For many of them, either safe and cost-effective treatment and/or preventive measures exist. However, many populations concerned lack access to these interventions and hence, NTDs are persisting. In settings with humanitarian crises resulting from natural disasters and climate change but also from armed conflicts the barriers to care are multiplied. As a consequence, poor health of the local, refugee and internally displaced people (IDP) populations is maintained, extending the vicious cycle of poverty.
Among the most important NTDs in Africa is schistosomiasis, a water-borne parasitic infection caused by the intermediate host snail-dependent blood flukes Schistosoma mansoni (intestinal schistosomiasis) and S. haematobium (urogenital schistosomiasis). Symptoms and signs include abdominal pain as well as blood in urine and stool with negative long-term impact on nutrition, growth and cognitive development. If left untreated, inflammation and chronic fibrosis resulting in organ dysfunction, liver enlargement, portal hypertension and bladder cancer may follow. While children and adults are affected alike, women and girls are particularly suffering from a complication of S. haematobium infection, namely female genital schistosomiasis (FGS). In FGS, inflammatory responses to parasite eggs trapped in the tissue cause extensive damage to the genital tract and reproductive organs, which can lead to ectopic pregnancies or infertility, increase the susceptibility to sexual transmitted infections (STIs) and HIV-1 and are associated with cervical cancer development.
Girls and women are at high risk
In sub-Saharan Africa (SSA), girls and women are at high risk of schistosomiasis infection due to exposure through domestic chores and limited access to treatment beyond school-based programs but also through their overall social status in predominantly patriarchal societies as it is the case in Chad. Epidemiological data on FGS is scarce, yet 56 million girls and women in SSA are estimated to be infected and face a double burden as they are also affected by stigma associated with the condition, impacting negatively on their physical and mental wellbeing. Knowledge and awareness of FGS in affected communities and among healthcare providers is low, requiring comprehensive information, education and communication in addition to training and support in clinical diagnosis and management.
WHO provides guidelines to national programmes for targeted schistosomiasis control, including FGS. These interventions entail mass drug administration (MDA) of praziquantel to school-aged children (SAC), combined with sensitization campaigns, risk reduction through environmental measures targeting the intermediate host-snails and improved sanitation infrastructure along with strengthening medical and curative capacity. WHO has set the goal to eliminate schistosomiasis as a public health problem until 2030. The WHO guidelines also call for intervention adaptation to each countries specific context, including the organisation of the health system, infrastructure and the consideration of cultural aspects to achieve a positive health impact. However, in fragile settings, these interventions are often interrupted or cannot be rolled out at all, leaving the treatment needs of refugees, IDP and the local population unattended. While many endemic countries can report tremendous progress, other countries like Chad could hardly initiate targeted schistosomiasis interventions.
Project objective
The aim of the ParaSahel – DIMAS project is to improve the health of refugees, IDPs and local population around Lake Chad with a special focus on schistosomiasis and women and girls. To do so, it relies on three innovative intervention approaches, all of which have been previously developed in the frame of competitively funded interdisciplinary research projects. The three innovative interventions are:
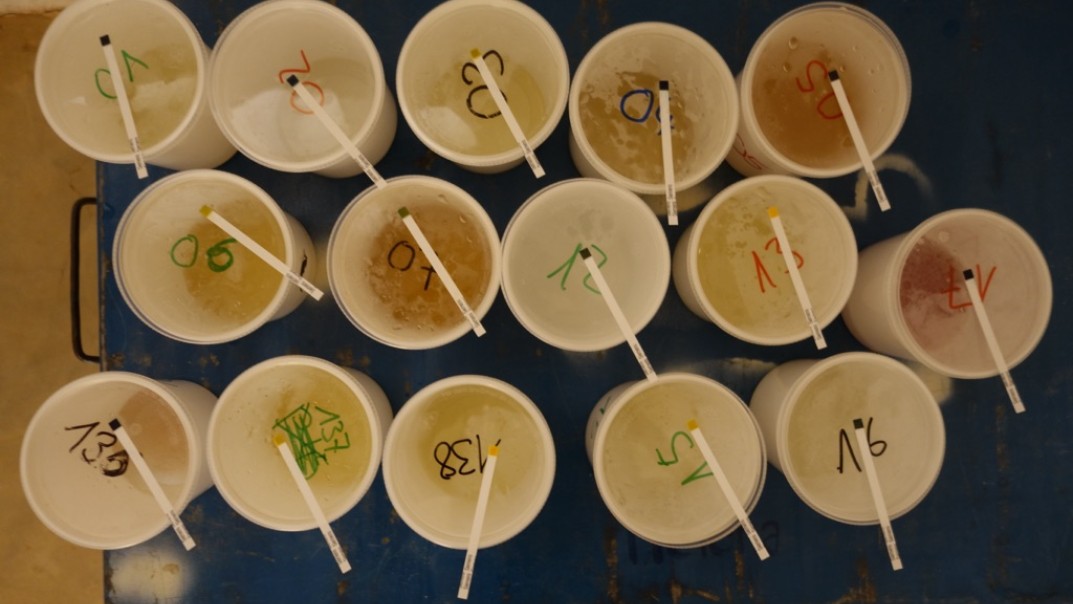
- At intervention level: Community co-designed, citizen science informed praziquantel MDA, covering all population groups
- At prevention level: Validated vocal health promotion messaging in local languages to an illiterate population through the locally developed health promotion app “BeAfya”, and
- At clinical care level: A digital clinical decision support system (CDSS) developed to serve specifically in humanitarian settings to improve child health and to be further validated in respect to improved diagnosis and treatment of urogenital conditions.
Often, novel, innovative tools and approaches elaborated in health research projects lack evidence for the feasibility and acceptability for scaling-up in the «real world». Here, the project wants to bring three existing, pre-tested tools into action. Together, they form a holistic multi-sectorial intervention through which it aims at achieving the following objectives:
- Improved acceptability and access to MDA, therewith increasing treatment coverage in a sustainable way.
- Increased knowledge and awareness of schistosomiasis and FGS symptoms, associated risks, prevention and treatment options among the community, health workers and health care providers through a locally developed, context adapted app delivering health promotion messaging in local languages.
- Improved diagnosis of paediatric and urogenital conditions including schistosomiasis and FGS in routine primary care serving the local, refugee and IDP population, with a special focus on women and girls, by training health staff in utilizing a CDSS tool
Project implementation
Integrating citizen science approaches and community participation processes will provide urgently needed learnings on how to empower the community to demand the health intervention and services needed, and strengthen the health system to deliver them. Therewith democratizing health research, intervention, prevention and services, the project bears the potential for advancing communities by increasing access to knowledge through citizen learning which can lead to social and – finally – systems change for better health.